Check out our entire series explaining the science involved in the coronavirus pandemic. Sign up to receive our coronavirus update each week.
Lately, you’ve probably been hearing a lot about a second wave of COVID-19 in the fall. You might be wondering, “When did the first wave end? Was I on vacation?”
The reality is the first wave hasn’t ended yet. We are still enduring the first wave and will be for some time to come. So why all the chatter about a second wave?
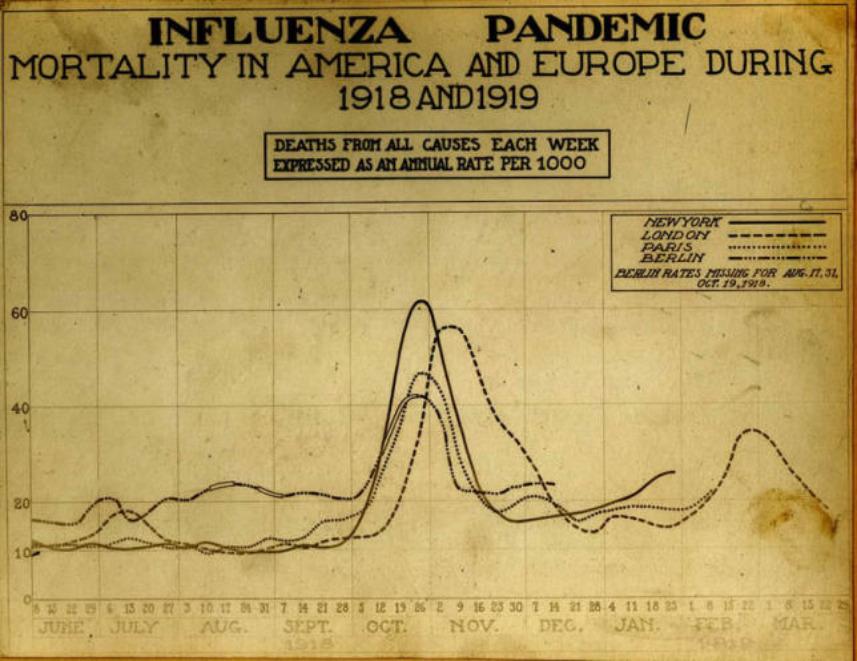
Well, since we have never seen anything like SARS-CoV-2 (the virus responsible for COVID-19) before, it’s tempting to look to past pandemics to predict the future. And the pandemic that seems the most relevant is the flu pandemic of 1918–19, sometimes inaccurately called the Spanish Flu. (Bonus question: Where did that name come from and why is it misleading?) Looking back on the spread of the flu in 1918, we see that there was a relatively small wave of flu in the spring of 1918, followed by a lull in the summer, followed by massive waves of the disease in the fall. It’s reasonable to wonder whether the same pattern could happen with COVID-19.
But let’s look more closely at the details. The spring wave of the 1918 influenza was not universal, few individual outbreaks spread to neighboring communities, and there were relatively few deaths. As you can see from the graph below, the spring wave barely registered as a blip of higher mortality in four major cities. In the fall, mortality rates tripled. When influenza broke out in a community in the fall of 1918, up to a third of the population would fall sick within just two weeks. Within a month, the flu would be gone, having killed 2 to 3 percent of those who fell ill. In many places, as in the case of London shown on the graph below, there was yet another wave of the virus in the spring of 1919.